Integrative Research
The Seaver Autism Center takes a unique genetics-first approach in ASD, which allows for highly coordinated preclinical and clinical studies. A major focus of the Center is Phelan-McDermid syndrome (PMS)/22q13 deletion syndrome, one of the more common single gene causes of ASD. At the Seaver Autism Center, we use a highly translational approach: we study patients with PMS, model PMS mutations in experimental models, and design and test novel pharmacological compounds based on study results in the experimental models.
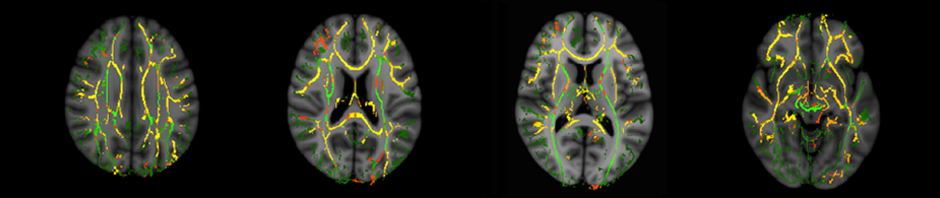
The behavioral and neurological features of PMS are due to mutation of the SHANK3 gene. Data indicate the SHANK3 pathway can be altered in ASD, even without a mutation in SHANK3. We aim to uncover the biological processes that are altered by SHANK3 mutations, so we can pharmacologically target these processes and alleviate the symptoms of the disorder. A powerful strategy to study the mechanisms underlying a disease entails the use of model organisms. Our preclinical research team is using both mice and rats carrying engineered mutations in SHANK3 as a model for PMS and for ASD. The consequences of SHANK3 deficiency in these models are then examined with a multidisciplinary approach, which includes molecular and cellular biology, electrophysiology, behavioral analyses, and neuroimaging. These analyses provide detailed knowledge of the biological changes that occur with the loss of SHANK3. This in turn identifies lead compounds for drug discovery that can be tested in the mouse or rat.
The clinical research team has translated findings from these preclinical models into experimental therapeutics for individuals with PMS. First, exciting results with Insulin-like Growth Factor-1 (IGF-1) treatment are reported below. As part of these studies, the clinical research team applies both neuroimaging and electrophysiology to investigate the effects of SHANK3 mutations on brain structure and function in humans. These studies also aim to identify biomarkers that can be used as outcome measures to evaluate the effects of behavioral or pharmacological forms of intervention. Moreover, through a joint effort by the preclinical and clinical research teams, we are collecting blood samples from subjects with PMS that can be used to derive nerve cells and to create a personalized experimental model for each patient. These models are an unparalleled tool for preclinical research and provide an exceptional preclinical model for drug development and screening.